Supplement Safety Regulations: Food vs. Pharmaceuticals
By Dilia Narduzzi
Supplements are big business. According to Grandview Research, the 2021 global dietary supplement market was valued at over 150 billion dollars, and it’s only projected to continue to grow in the coming years. By 2030, the market is estimated to be worth over 300 billion.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 outlines what exactly a dietary supplement is, according to the FDA: “The ‘dietary ingredients’ in these products may include: vitamins, minerals, herbs or other botanicals, amino acids, and substances such as enzymes, organ tissues, glandulars, and metabolites … They can also be in other forms, such as a bar, but if they are, information on their label must not represent the product as a conventional food or a sole item of a meal or diet,” the latter of which means that “a supplement cannot be a meal replacement,” says Tara Couch, Ph.D., Senior Director of Dietary Supplement and Tobacco Services at EAS Consulting Group.
You may be surprised to learn, though, that supplements are classified under the FDA jurisdictions with regard to foods, not drugs, and that the lead narrative around supplements is that they are largely unregulated.
While many people take a dietary supplement for their purported health benefits, you may already know that supplement labels cannot make disease claims, like, for example, that the product therein can cure Covid-19 or treat cardiovascular disease. You may be surprised to learn, though, that supplements are classified under the FDA jurisdictions with regard to foods, not drugs, and that the lead narrative around supplements is that they are largely unregulated. Let’s dive into what’s going on here, since, like a lot of things, the truth is a little more complicated.
“Dietary supplements are a weird duck,” says Couch. In fact, says Couch, who has a background in both the pharmaceutical industry and the dietary supplement industry, “there are extensive regulations for dietary supplements.” Part of the confusion comes in because there is no separate “centre of dietary supplements” at the FDA, like there is with food, tobacco, and drugs. There is an office of dietary supplements at the FDA in the food department, but no designated centre. “Dietary supplements got classified as food” under the DSHEA passed by Congress, says Couch, and via that legislation supplements are allowed to make structure/function claims, which are different than disease claims (a structure/function claim is something like “fiber maintains bowel regularity,” according to the FDA’s website), and which is also something that differentiates a supplement from a food.
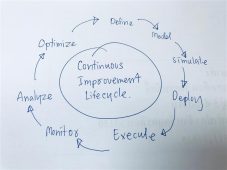
Additionally, while dietary supplements do not need to gain a formal pre-approval before going to market, like a drug would, in 2007, the FDA implemented what’s called “good manufacturing practices” for dietary supplements, says Couch, and these rules “do not at all look like food regulations. They look like drug regulations.” Later in 2007, rules were passed that any adverse events caused by a dietary supplement needed to be reported to the FDA, which is similar to the rules followed by the pharmaceutical industry. A lot of these rules were by design and with the consumer in mind, to get products out more quickly than a drug and at lesser expense than a drug that needs extensive pre-approvals, says Couch. All supplement companies are supposed to be adhering to rules about labelling, structure/function, and manufacturing when their product goes to market. The problem comes in because the office of dietary supplements at the FDA doesn’t have the budget to closely monitor such a burgeoning industry. The industry has boomed over the last decades since DSHEA, but the FDA’s budget hasn’t much increased. Officers do inspect facilities and, on average, pre-Covid, they inspected “over 1700 facilities a year,” say Couch, though that number has been down during Covid. “But even 1700 observations aren’t that many given the size of the dietary supplement industry,” says Couch.
Issues can arise when you buy something—whether it’s a cinnamon tablet, or a product containing green tea extract—for their purported health benefits, as a supplement to your diet. How do you know the product is doing something? That it is safe to consume? As the industry stands, there aren’t “great ways to know the product you’re buying is going to have the effects you want on your body—that’s called efficacy,” says Ashley Moyna, a registered dietitian and Marketing & Operations Manager at Canomiks Inc., a technology company using AI and genomics to ensure the safety and test the efficacy of dietary supplements and functional food.
The FDA does not approve dietary supplement products for safety and effectiveness before they are sold. Instead, dietary supplement manufacturers and distributors are responsible for ensuring their products are safe before being marketed, but companies only need to share the safety testing information with the FDA if their products are reported as adverse events or if their product uses a new dietary ingredient, says Moyna.
Because the FDA doesn’t require pre-approvals, as described above, “companies don’t have to do efficacy testing or report their safety data and evidence to the FDA before the product hits shelves,” says Moyna.
Products are pulled once they become problematic, says Moyna, when adverse events are reported, which is a part of what’s called post-market regulation. It’s a bit of a catch-22 because, yes, “if there are problems, they are pulled off the shelves,” but even if there aren’t overt adverse events, “it doesn’t mean that everything in a product is proven to work,” says Moyna. Supplements can also interact with pharmaceuticals in some cases, so checking with a healthcare practitioner before taking them is also always advised, which shows the gray area of supplements classified as food, because you likely wouldn’t need to do that if you decided to start consuming more broccoli, for instance.
Where does all of this leave us? “There are a lot of companies doing really great work and there is a lot of opportunity in this space,” says Moyna, but consumers should still know the basics of this industry before they buy. Just because a product is sitting on the shelf, that doesn’t immediately mean it has been extensively tested for safety. Because of the FDA’s limited budget, even bad actors sometimes get away with non-compliance for years, blighting all of the good companies doing their jobs of “voluntary compliance” to the FDA’s regulations, says Couch. In these cases, a stronger, faster message needs to be sent so that bad players know they need to clean up their acts. “I have a colleague who says, ‘You’re not making a widget, you’re making something that’s being ingested,’” says Couch, “something that’s expected to impact the structure and function of someone’s body, so there should be some heightened responsibility there.”
About the author:
Dilia Narduzzi is a freelance writer in Hamilton, ON. She’s written for Costco Connection Canada, Canadian Grocer, The Women’s Brain Health Initiative, Country Guide, Maclean’s, and other venues. She writes on health, food, agriculture, and books.
-
 FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
-
 FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
-
 FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
-
 GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
-
 FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
-
 FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants
FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants




