Chickening out on Campylobacter in the UK: More Progress Needed
By Suzanne Osborne, Ph.D
If every UK chicken contaminated with Campylobacter went to a football game today, you could fill Wembley Stadium, an arena with a 90,000-person capacity, over 7,200 times.
The UK Research and Innovation Strategy for Campylobacter (RISC) took aim at the most serious cause of food-borne illness in the United Kingdom. Campylobacter sickens more than 300,000 people each year, and sends 15,000 of them to hospital for treatment. About 80 people die from the illness every year in the UK.
Highest Level of Contamination
“Health officials are highly motivated to find a solution.”
RISC was supposed to assist the £85 billion poultry industry by focusing on birds with the highest level of contamination: those with more than 1,000 bacteria for every gram of chicken. In 2010 it set an ambitious goal to reduce contamination levels to 10%.
Although news reports suggest significant leaps were made, highlighting that only 9.5% of retail chicken had the highest levels of contamination at the end of 2015, a closer look reveals that monitoring methods changed over the course of the project and retailers had started removing the carcass neck skin from their product. This is the most highly contaminated part of the chicken. If we include neck skin in the analysis, the levels of contamination are closer to 19.7%. That is still 1,900 sold out games at Wembley Stadium.
Slaughter houses did even worse, only managing to reduce contamination levels to 23%. Representatives at Food Standards Scotland (FSS) reflected that, “The target was ambitious, and we were disappointed that it was not achieved by the end of 2015.” They further note that, “Campylobacter reduction will remain a priority until it ceases to be a public health issue.”
No Single Solution
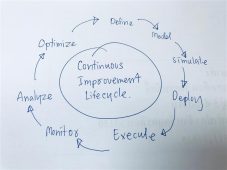
It is impossible to pinpoint why the RISC target was not achieved. The FSS emphasizes that, “there is no single solution or ‘silver bullet’ for eliminating the pathogen [and], control will be reliant on a number of different intervention approaches being applied throughout the food chain.”
Back in 2008, prior to the RISC project, members of the poultry industry, in the areas of retail, research, and production, identified multiple intervention points to tackle Campylobacter. Theychose to focus on improving farm and processing biosecurity by implementing new standards, decontaminating carcasses through rapid surface chilling, and lobbying government to enable the use of antimicrobial treatments in processing plants.
A Vaccine is Needed
A mid-term RISC meeting, held in 2013, reflected the fact that on-farm measures had had little effect on Campylobacter levels: there was a large non-compliance rate. With doubts raised on the effectiveness of on-farm controls, RISC’s attention turned to processing. Processing interventions, though they hold the promise of short-term results, seem at odds with the fact that most contamination comes from the chicken as a whole (50-80%) rather than from post-harvest activities (20-30%). Due to the prevalence of Campylobacter in the environment, the reality is that eradication of the pathogen on the farm will be difficult without the development of a vaccine. Knowledge about environmental sources of the bacteria, seasonal effects, and human behaviours that impact uptake of new recommendations would greatly benefit attempts to reduce contamination on the farm.
Moving forward, the FSS and Food Safety Authority (FSA) continue to meet regularly with the major retailers and poultry companies in the UK. They plan to continue to publish survey data onCampylobacter in fresh chicken at retail and they are committed to data transparency. Although the RISC fell short of its original goals, the alliance of industry, producers, processors, and retail has made gains towards reducing Campylobacter numbers in poultry and continues to serve as a model collaborative effort in food security across the globe. Aside from the obvious human impact of Campylobacter, the cost of treating it runs to in excess of £583 million annually in the UK. Health officials are highly motivated to find a solution.
About the Author
Dr. Suzanne Osborne is a Research Fellow at the SickKids Hospital in Toronto. Her expertise is in the field of host-pathogen interactions and foodborne pathogens. She has received numerous awards and is currently funded by the Banting Research Fellowship.
-
 FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
-
 FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
-
 FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
-
 GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
-
 FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
-
 FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants
FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants




