Antibiotics and the Food Industry
By Suzanne E. Osborne, PhD Candidate
The antibiotic era is at an end. Widespread resistance to these once heralded miracle drugs has shattered our ability to treat infectious disease. As we scramble to save existing antibiotics, criticism has targeted agriculture given their large consumption of antibiotics for non-medicinal purposes. The policies and practices implemented in the food safety industry will be key players in whether we are able to salvage these drugs for medicinal purposes. A clear understanding of the nature of antibiotics and resistance is needed for those invested in food safety.
What is an Antibiotic?
Antibiotics are small chemicals that function to kill or inhibit the growth of microorganisms by inhibiting essential functions. Although antibiotics were originally isolated naturally from soil-dwelling microorganisms, many are now synthetically produced. The most common natural producers of antibiotics include the molds Penicillium and Cephalosporium and a family of bacteria called Streptomycetes.
How do Bacteria Resist Antibiotics?
Bacteria can modify themselves through mutation so that the antibiotic no longer recognizes the molecule it targets. Many bacteria assemble pumps that expel drugs. Antibiotic efficacy can be lost through bacterial-mediated degradation or chemical alteration. Bacteria can also modify their surrounding protective membrane barrier, making it more difficult for the drug to access its target. These mechanisms of resistance are encoded within the cell’s genetic material (DNA) and are therefore inheritable.
Where did Antibiotic Resistance Come From?
Most antibiotics come from microorganisms themselves. The original purpose of these chemicals was in competition: a bacterium could release a chemical to destroy neighboring bacteria competing for the same resource. In order to prevent killing themselves, any antibiotic-producing organism would necessarily have resistance to the antibiotic it produces. Resistance is therefore a naturally occurring phenomenon. How then does resistance move from a relatively harmless, antibiotic-producing soil bacterium to a medically relevant human pathogen? Bacteria naturally harbor the ability to freely exchange genetic information (DNA). Thus, bacteria can literally ‘donate’ resistance to each other.
The overuse of antibiotics in medicine and agriculture has created a ‘do or die’ scenario. Organisms that have acquired resistance survive in the presence of these drugs and sensitive bacteria are killed. Over time, resistant bacteria replace the natural, drug-sensitive populations.
What is Being Done to Find new Antibiotics?
Researchers are isolating microorganisms from unique and often unexplored environments trying to discover new antibiotics. Others try to structurally modify existing drugs so that they retain efficacy but ‘look’ different to the bacteria. Our knowledge of survival and infection strategies used by bacteria now allows scientists to screen massive collections of synthetic chemicals looking for potential inhibitory drugs. Some invest in preventative strategies such as vaccine development and treatments that boost our own immune system (i.e. probiotics).
The Controversy
Use of antibiotics for growth promotion in livestock is directly linked to the emergence of antibiotic resistant bacteria isolated from animals. In addition, increasingly resistant bacteria can be isolated from animal meat products. It seems logical to assume that the use of antibiotics in animal feed therefore drives the emergence of resistance in human medicine. However, observations that resistance ‘profiles’ vary between animal and human bacterial isolates has led many to question this assumption. In reality, it is difficult to directly trace resistant bacteria from animals to foodstuffs to humans. In addition, banning growth promoting antibiotics increases the use of more medically relevant drugs to therapeutically treat sick livestock.
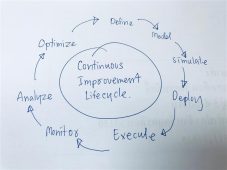
Ideas on ‘solutions’ to the antibiotic crisis vary with proposals ranging from mild restrictions to outright banning of drug use in agriculture. It is critical that the food safety industry remains informed of policies being implemented in their own countries as these decisions will affect all levels of safe food preparation.
References
(1) Alekshun, M.N. and Levy, S. B. Molecular mechanisms of antibacterial multidrug resistance. 2007. Cell 128: 1037-1050
(2) Phillips, I., et al. Does the use of antibiotics in food animals pose a risk to human health? 2003. J. Antimicrob. Chemo. 53: 28-52.
About the Author
Institute for Infectious Disease Research, Department of Biochemistry and Biomedical Sciences, McMaster University, Hamilton, Canada.
SEO is funded by the Canadian Institute for Health Research (CIHR) and is a recipient of the prestigious Canadian Vanier Scholarship.
To have more articles like this emailed to your inbox, become a GFSR Member today!
-
 FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
-
 FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
-
 FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
-
 GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
-
 FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
-
 FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants
FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants



