The Sobering Danger of Mycotoxin Cocktails
By: Suzanne Osborne, PhD
When determining whether a driver of a motor vehicle is impaired, the number and type of drinks they have consumed is taken into consideration, not just the alcohol content of a single drink. So why do food safety regulations fail to recognize the interaction of co-occurring mycotoxins?
Mycotoxins are toxic chemicals produced by fungi (commonly known as moulds) that can grow on crops before or after harvest. Foods that are often affected include cereals, nuts, fruit (fresh and dried), coffee, cocoa, spices, oilseeds and milk.
When people eat foods contaminated with mycotoxins they can quickly begin vomiting or haemorrhaging. In many people, the symptoms of mycotoxin consumption can appear years later as, for example, an impaired immune system or cancer.
Most mycotoxins are chemically very stable, which means they can linger in food long after mould is gone. Contaminated food can be present at any stage of production, putting consumers and businesses in the food supply chain at health and economic risk, respectively.
The U.S. Food and Drug Administration (FDA) estimates $932-million worth of produce is lost annually due to mycotoxin contamination. As climate change provides increasingly favourable temperatures for mould growth, this number is expected to increase. There is a high chance that benign mycotoxins (can) become health hazards.
While there are hundreds of known mycotoxins, only a small number are regulated by food safety guidelines because of their high level of toxicity. Common mycotoxins include (but are not limited to) aflatoxins, ochratoxin A, patulin, fumonisins, patulin and zearalenone. These are so toxic that even trace amounts can be hazardous to human health. Consequently, diagnostic strategies must be highly sensitive.
Simple, high-throughput, colour-change based ELISA (enzyme-linked immunosorbent assay) tests have traditionally been used by food scientists to detect toxin levels down to 0.1 parts per billion. The development of biosensors have increased sensitivity to 0.03 parts per billion yet only a few are commercially available. Both methods are limited because they generally only detect a single mycotoxin.
Recently, food scientists have turned to high-pressure liquid chromotography (HPLC) combined with mass spectroscopy (MS) to quickly identify hundreds of toxins in a single sample with sensitivities down to 0.01 parts per billion.
Although the use of HPLC-MS requires a degree of technical expertise, this analytical chemistry tool is advantageous since food is commonly contaminated with multiple mycotoxins. It turns out that the toxicity level of a mycotoxin can be increased when other toxins are present in the same food. For example, fuminocins have been shown to enhance the ability of aflatoxin to cause tumors. This combination effect often occurs when multiple mycotoxins target similar cellular machinery. This process is known as the mycotoxin cocktail effect.
At present, food safety regulations are based on the toxicity of an individual mycotoxin even though there is evidence that actual toxicity levels depend on this cocktail composition. As a result, there is a pressing need for government to assess the risk of synergistic mycotoxins and revise food safety regulations accordingly. There are also hundreds of mycotoxins that are ignored by regulations altogether because, individually, they do not cause human illness.
“To date, not many studies have focused on synergistic interactions beyond the main regulated mycotoxins … (and) other mycotoxins have not been toxicologically tested individually,” says Dr. Rachael Clark, a mycotoxin expert at the Institute for Global Food Safety in Northern Ireland, U.K. “There is a high chance that benign mycotoxins (can) become health hazards in combination … (which has) implications for food safety.”
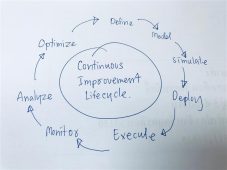
In the meantime, it is essential businesses in the food supply chain become aware of the risk of mycotoxin cocktails and implement detection strategies that identify multiple mycotoxins simultaneously to inform decision-making.
About the Author
Dr. Suzanne Osborne’s expertise is in the field of host-pathogen interactions and foodborne bacteria. She obtained her doctoral degree at McMaster University and worked as a Research Fellow at the Hospital for Sick Children (Toronto). She has received numerous awards for her research. Suzanne currently does freelance science writing and grant writing.
To have more articles like this emailed to your inbox, become a GFSR Member today!
-
 FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
-
 FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
-
 FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
-
 GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
-
 FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
-
 FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants
FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants



