Know Your Enemy: Escherichia coli, E.coli
By: Suzanne Osborne, Ph.D
Escherichia coli (E. coli) is the most commonly known food-borne pathogen. Due to its ease of growth and genetic manipulation in laboratory conditions it is also the most intensely studied bacteria in biomedical research, acting as a model for our understanding of microorganisms. Often synonymous with fear, the designation “E. coli” actually covers a broad spectrum of bacterial subtypes with diverse effects on human health. This variability is highlighted by the fact that the entire E. coli species shares only 20% genetic identity. Most E. coli are non-pathogenic, often residing as beneficial commensals within the intestine where they can even act to prevent infection. The human gut, which can carry 1,000,000 E. coli cells per gram of feces, is colonized by these commensal E.coli strains within the first 48 hours after birth.
E. coli is often categorized based on the clinical diseases it causes which are outlined in the table below.
| Name | Disease |
|
Enteropathogenic E. coli (EPEC) |
Common cause of diarrhea. Use adhesive molecule called intimin to attach to intestinal cells. The resulting effacement of the intestine causes diarrhea. May possess toxins. |
| Enterohemorrhagic E. coli (EHEC) | Highly infectious. Colonizes the lower part of the intestinal tract. Can cause haemorrhagic colitis (bloody diarrhea) and the potentially fatal haemolytic uraemic syndrome (HUS) and kidney failure. Produces Shiga toxin. |
| Enterotoxigenic E. coli (ETEC | Causes travellers diarrhea. Produces the LT and ST enterotoxins. Common cause of diarrhea in developing countries. |
| Enteroinvasive E. coli (EIEC) | Causes watery diarrhea and high fever. |
| Enteroaggregative E. coli (EAEC) | Common cause of travellers diarrhea. Uses fimbrea appendages to stongly adhere to the cells of both small and large intestine. |
| Uropathogenic E. coli (UPEC) | Causes urinary tract infections. |
The estimated incidence rate for EHEC ranges from <1 to 22 cases per 100,000 people depending on the region. EHEC is particularly dangerous owing to its production of the Shiga toxin. Shiga toxin binds to a particular receptor molecule (Gb3) expressed on cells lining the intestinal tract. Once bound, Shiga toxin eventually leads to the death of the intestinal cell. This causes severe cramping and bloody diarrhea. Although most patients recover within 10 days, 10% of people will develop the potentially fatal haemolytic uraemic syndrome (HUS) which can lead to rapid
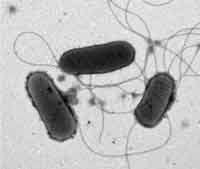
Transmission Electron Microscopy Image – 20,000 x magnification, image of 3 bacteria (grey rods) with their attached flagella (used for swimming) (grey threads)
kidney failure. This is due to the additional expression of Gb3 on kidney (renal) cells. It is estimated that 65-85% of cases of EHEC result from exposure to contaminated food. Ruminants, such as cattle, are the most common reservoir of EHEC which transmit the pathogen by fecal contamination. EHEC cannot cause disease in cattle, swine or some other ruminants since these animals do not express the Gb3 receptor. Shiga toxin is not produced exclusively by EHEC; the June 2011 outbreak of E. coli in Europe appears to be the result of an EAEC strain that has acquired the Shiga toxin. Treatment of infected persons is highly controversial since evidence suggests that antibiotic treatment can actually increase the production of Shiga toxin.
The most common sources of contaminated foods are undercooked ground beef and raw milk. Although there are increasing incidences of contaminated water, fruits and vegetables, these are generally believed to result from cross-contamination on surfaces during processing or from contact with fecal matter at some point during cultivation. Evidence does not yet suggest strategies to limit contamination at the farm level although it has been suggested that pre-slaughter screening or treatment may decrease cross-contamination. The recommended best defences against E. coli include hygienic handling and cooking at the production and consumer level respectively.
References:
World Health Organization. Fact Sheet: Enterohaemorrhagic Escherichia coli (EHEC). http://www.who.int/mediacentre/factsheet/fs125/en/
Kupferschmidt, Kai. Scientists Rush to Study Genome of Lethal E. coli. Science, 2011. 332(6035):1249-1250.
About the Author
Dr. Suzanne Osborne’s expertise is in the field of host-pathogen interactions and foodborne bacteria. She obtained her doctoral degree at McMaster University and worked as a Research Fellow at the Hospital for Sick Children (Toronto). She has received numerous awards for her research. Suzanne currently does freelance science writing and grant writing.
To have more articles like this emailed to your inbox, become a GFSR Member today!
-
 FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
FeaturedRisk management
The Cost of a Breach: What a Cyberattack Could Mean for Food Safety Recalls
-
 FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
FeaturedRisk management
Securing the Food Chain: How ISO/IEC 27001 Strengthens Cybersecurity
-
 FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
FeaturedRisk management
Revolutionizing Food Safety Training: Breaking Out of the “Check-the-Box” Mentality
-
 GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
GFSI Standards
GFSI 2025: Building Trust, Tech-Forward Solutions, and Global Unity in Food Safety
-
 FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
FeaturedFood Safety
Integrated Pest Management: Strategies to Protect Your Brand’s Reputation
-
 FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants
FeaturedFood Safety Culture & Training
No Open Door Policy: Challenges That Impact Pest Control in Food Processing Plants



